Health Net News Now

February 2026
NABIP CEO Roundtable 2026 – Come join us for an industry discussion!

This year's CEO Roundtable is your chance to hear directly from the individuals influencing the policies, strategies, and innovations that impact Oregon’s benefits market. Come be part of a forward-looking conversation focused on practical insights and real-world solutions.
When:
Wednesday, January 28, 2026
10:00 a.m. to 12:00 p.m. Pacific time
2026 CEO Roundtable Panelists
Christina Jackson, Health Net of Oregon
Moderator
Tom Holt, NABIP Oregon Lobbyist
Health Care Industry Expected to See Oregon's Greatest Job Growth Over Next Decade

From Oregon Public Broadcasting (OPB) 12/25.
Oregon's private health care and social assistance sector is expected to add 40,400 jobs over the next decade, making it the fastest growing industry according to the latest projections from the state's Employment Department. Overall, the state's total employment is projected to increase by a modest 140,600 jobs, or 6%, by 2034.
"Nearly all broad sectors of Oregon's economy are expected to add jobs over the decade," Sarah Cunningham, Oregon's projection economist, said in a video news release. "The exception is federal government, which is projected to see a slight decline in jobs. Private health care and social assistance is expected to add the most jobs by 2034." That represents a 13% growth rate, Cunningham said, meaning three out of every 10 new jobs added will be in health care and social assistance. Longer life expectancies, Oregon's aging population and long-term population growth are all expected to contribute to the growing need for health care workers in the state.
Oregon Health Authority to Allow Trillium to Take Over Serving Lane County PacificSource Members

The Oregon Health Authority says insurer Trillium will take over 90,000 low-income patients served by PacificSource in Lane County.
Springfield-based PacificSource announced last month it would not renew Lane County's Medicaid contract, citing financial losses and low rates.
In Oregon, private companies contract with OHA to provide Medicaid to low-income people. Companies that provide that service are called Coordinated Care Organizations, or CCOs.
OHA Policy and Programs Director Dave Baden said the agency is negotiating with PacificSource to extend its contract to February, when it hopes Trillium will take over.
"The most important thing is, we're trying to build in as much time for as smooth a transition as possible," Baden said. Baden said Trillium, which serves around 30,000 Lane County residents now, has assured the agency it will expand its provider network to care for additional patients.
"We obviously want to see as robust a network as possible and really encourage all providers to try to be in the Oregon Health Plan and serve Medicaid members," Baden said. "Ultimately, those decisions are business decisions between Trillium and the contracted providers."
Which Urgent Care Clinics in Lane County Accept Trillium?

As Trillium Community Health Plan transitions approximately 96,000 Oregon Health Plan members from PacificSource beginning February 1, many members are asking where they can receive covered urgent care services in Lane County.
Here's a quick guide originally published in the Register-Guard, that lists urgent care options that do—and do not—accept Trillium.
When to Use Urgent Care vs. the Emergency Room
Urgent Care is appropriate for non-life-threatening issues such as:
- Minor injuries or burns
- Asthma flare-ups
- Cuts requiring stitches
- Skin conditions or infections
Emergency care is needed for symptoms like:
- Chest pain
- Trouble breathing
- Severe bleeding
Emergency departments are available throughout Lane County and must provide care regardless of insurance status, as required by federal law.
For more information about the Trillium transition and covered services, contact your Health Net Account Representative.
Sharecare Wellness – A New Year Means New Wellness Incentives and Programs

Steps to Take for a Healthier You
Choose the tools, resources and programs that work for you! They come with our plans at no extra cost. Looking for the best way to reach your health goals? Log in to your account to access these programs and services to help you and your family stay healthy.
Your First Step:
Take the RealAge Test (Health Assessment)
The RealAge Test provides members with a personalized report of behavioral and medical health risks. Immediately after taking the online RealAge Test, members will receive a personalized action plan.
Wellness Rewards Program
Get up to $100 in rewards! Take the online RealAge Test (health assessment) and share the results with your primary care physician to earn a $50 gift card. Learn how you can earn up to $50 more (PDF).
Visit our Health Net Wellness Center page for more information.
Who Was St. Valentine?
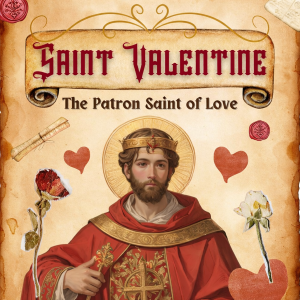
This year, Valentine's Day falls on Saturday, February 14.
Across the United States and around the world, people will exchange candy, flowers, and gifts in the name of St. Valentine.
But who was this mysterious saint, and where did these traditions begin?
The history of Valentine's Day is steeped in mystery, blending Christian and ancient Roman traditions. The Catholic Church recognizes at least three martyrs named Valentine or Valentinus.
One legend describes a third-century Roman priest who secretly married couples after Emperor Claudius II banned marriage for young men. When discovered, Valentine was executed. Another story points to St. Valentine of Interamna, a bishop beheaded for refusing to renounce his faith.
Other legends claim Valentine was killed for helping persecuted Christians escape Roman prisons. One popular tale says he sent the first "valentine" to a young woman—possibly his jailor's daughter—signing it, "From your Valentine."
Though the true story remains unclear, these legends portray Valentine as a heroic and romantic figure. By the Middle Ages, he had become one of the most popular saints in England and France.
For more interesting Valentine's Day facts and traditions, visit History.com
Have a Happy Valentine's, Galentine's, Palentines –
However You Celebrate!
